THERE HAVE been countless information campaigns and seminars that debunk medical myths surrounding the human immunodeficiency virus (HIV) such as misconceptions about how the disease gets transmitted. However, there is more to a person living with HIV than health-related issues—the virus permeates one’s deepest thoughts on their relationships and self-esteem, which then emphasizes the importance of having a supportive community that can see beyond labels.
HIV is a virus that attacks CD4 cells, which fight off infections to help safeguard the immune system. If left untreated, HIV will continue to destroy CD4 cells and make the body less able to fight off diseases or cancers. Though it can’t be transmitted through saliva, the virus can be contracted through the exchange of blood, semen, and anal or vaginal fluids during sexual intercourse. It can also be transmitted through sharing needles and syringes, pregnancy, and breastfeeding.
There’s no cure for HIV just yet, but those with HIV can still live regular life spans through medication. Untreated HIV can develop into acquired immunodeficiency syndrome (AIDS), the final stage of HIV where the immune system is severely weakened. Though the progression of AIDS can be delayed with medication, those left untreated often pass away two years after the onset of AIDS.
Emmanuel*, a Filipino university student, has been living with HIV for two years now, and he continues to battle the apprehensions that come with his condition.
Foreshadowed fate
He remembers the details about the day he was diagnosed as HIV-positive quite clearly. The date? November 29, 2017. His age? 17-years-old and and just about to graduate from high school. “I doubt I can ever forget [that day],” Emmanuel says.
But Emmanuel already had an inkling about his illness even before the diagnosis was handed to him. There were a few tell-tale signs: First, he was sexually active; second, his health had been declining—he had flu-like symptoms more frequently, experienced some skin problems like rashes and skin asthma, and suffered from alarming body temperatures whenever he got sick.
These symptoms prompted him to seek out medical help, but heading to a clinic an HIV test isn’t as simple as it sounds. Emmanuel’s suspicions had already rattled him, but he had to face another equally terrifying task: Having to tell his parents. At the time of his testing, minors weren’t allowed to get tested without their parents’ consent. It is now possible in the Philippines today, but Emmanuel didn’t have that opportunity.
“I was scared to tell them, but then they found out one way or another that I was sexually active. Then they noticed the drop in my health, and they pretty much ordered me to get tested,” he explains.
An unveiling
The results were in a sealed, white envelope. The nurse handed it to Emmanuel, who was accompanied by his sister. With shaking hands, he took some time to finally open what seemed like his fate.
He didn’t even need to read the whole thing. His eyes were immediately drawn to that ominous phrase: Positive for HIV. Like a scene in a movie, it was as if all sound in the room had gone dull. Time froze, and all focus was directed to those three printed words.
Emmanuel didn’t cry. He just stared. It was his sister who had to hold back tears.
After he called his parents to tell them the results, his father cried through the phone. It still wasn’t hitting Emmanuel. It was when he had to personally tell his friends that it all came crashing down: “[When] I saw them crying, it really hit me like—oh God. I cried. My friends were crying.”
Daily battles
The first six months after his diagnosis were spent dealing with the declining condition of his health. His CD4 count, a measure of the white blood cells that the HIV virus targets, was still well below the average of 500 to 1400 cells per microliter of blood—a risky amount of only 70 cells per microliter. His viral load also remained in the thousands at 9000 per milliliter, putting him at a greater risk of contracting infections and illnesses due to his weakened immune system. Then, there was the suspicion that the virus was already resistant to some of the medicines he was taking. He had no choice but to get the virus genotyped to determine if it was resistant to antiretroviral therapy, the recommended drug treatment for those diagnosed with HIV.
At this time, Emmanuel had to make some small lifestyle changes to protect himself while his immunity was low. First, he had to wear face masks all the time—even at home.
Second, he had to be wary of his hygiene. Carrying around alcohol was necessary. Utensils from other restaurants were also a risk, and he needed to ensure that what he used was cleaned thoroughly. His utensils at home were also marked with masking tape so that no one else would use them.
Third, he had to avoid exercise and religiously monitor what he ate to make sure he was getting enough nutrition. Emmanuel wasn’t allowed to engage in sports anymore, and he had to put a stop to all his club activities. After school, he had to go home immediately. Even commuting wasn’t safe as it meant being exposed to pollutants and other people.
“I was protesting because [not commuting] was expensive, but then they told me that me getting sick would be more expensive if I had to be sent to hospital,” he says.
Thoughts for company
Eventually, the time came for Emmanuel to get his virus genotyped. There are only two facilities in the Philippines that can facilitate the genotyping procedure: The National Institute of Health in the University of the Philippines Manila (UPM) and the Research Institute for Tropical Medicine in Muntinlupa.
Emmanuel decided to go with UPM. It was relatively nearer compared to Muntinlupa and the services they offered were less expensive since it was a public institution. It was the lesser of two evils, and there wasn’t much other choice than to get his virus genotyped as soon as possible.
Unfortunately, his parents and siblings had taken enough work leaves and weren’t able to accompany him to this nerve-wracking visit. “I then asked my best friends, but they also weren’t available,” Emmanuel said.
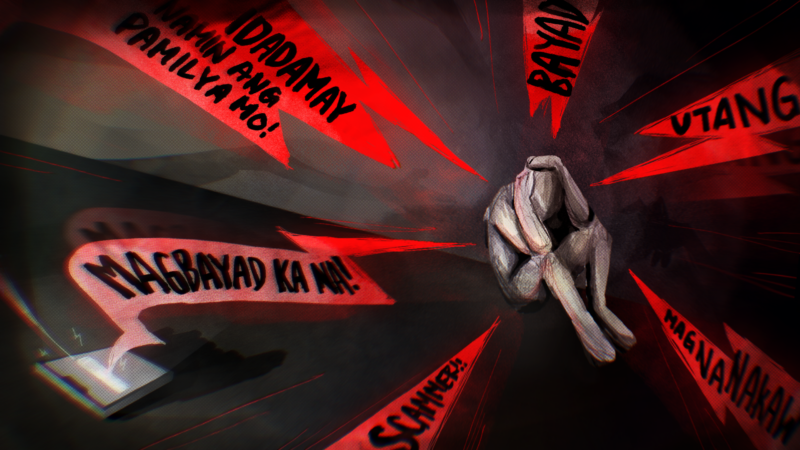
Ironically, even though his health was stable and the genotyping was purely for figuring out what medicines he had to take, Emmanuel felt a different kind of illness within him. It was a toxic blend of anxiety and despair: What if the virus is already resistant to all the common medications? What if I have to resort to experimental drugs?
What will happen to me?
These were questions he had to face alone, with no one else to share his worries with—there is nothing scarier than having to be in a muddle of panic, fear, and paranoia when you’re on your own.
The ride to UPM was a bleak and lonely trip to a very decisive discovery about his health.
Emmanuel ended up paying over Php 12,000 for three tests during that month: A CD4 count, a viral load test, and the HIV genotyping in UPM. He can still remember the fear he felt upon hearing that the virus was already resistant to almost 10 different medications.
Beyond illness
Today, Emmanuel’s viral load is undetectable. It has been two years since his diagnosis and the restrictions of Emmanuel’s lifestyle have become more lenient: His parents now allow him to go to parties and even hang out with friends. He no longer needs to wear a face mask everywhere as long as he takes his daily medication and goes for occasional checkups at the hospital. The worries that his family once had for him and his health have lightened up, and Emmanuel feels that he can enjoy aspects of his life that he felt he had lost when he was diagnosed. Things have gone back to normal, save for a few restrictions on his diet that limited his intake of fatty foods, alcohol, and anything that could potentially damage his liver.
Though his health has stabilized, the feelings of anxiety and low self-esteem still linger. There is always the question of whether or not he will find a partner who will accept him for his condition.
“Say I wanted to marry this girl. We won’t be able to have children because there’s a huge risk. Even now that [my HIV] is undetectable and non-transmissible, there’s still a risk of me passing on the virus to her and a baby. So how can we have a kid? There’s always adoption, but for some people [a biological child is] an important factor for them,” Emmanuel laments.
Even with a male partner or if children weren’t a factor, there is always some risk of transferring the virus through sexual intercourse. Aside from that, there is still some stigma surrounding HIV and people who live with it. This pushes people like Emmanuel to have intrusive thoughts and doubt their own self-worth: How can anyone accept me as a partner if I have this sickness?
Fortunately, the people in Emmanuel’s life have been supportive. Knowing that he has this lifetime illness changed his perspective on life. Now, Emmanuel tries as much as possible to spend more time with his loved ones. “I don’t want to resent anything, I just want to be able to express my love [during] my lifetime,” he says.
In Emmanuel’s case, a huge part of discovering and dealing with the fact that he had to live with HIV was the fear of what others would think of him. And yet, he took that gamble and trusted the people around him. Emmanuel’s friends and family helped him manage his condition, proving just how a community that looks beyond labels can help overcome any doubts and fears. Confiding in even just one person—someone you absolutely trust—can make a world of difference.
*Editor’s note: The name of the interviewee has been changed at their request in order to protect their identity and privacy.